Diarrea crónica en gatos means loose or watery stools that persist for 3+ weeks (or keep returning). It isn’t a diagnosis by itself—chronic diarrhea usually signals an underlying issue such as parasites, diet intolerance, inflammation (IBD), infection, or (especially in older cats) conditions like hyperthyroidism or kidney disease.
In this guide, you’ll learn what the stool pattern can tell you, what vets typically test for, and safe, practical home support while you’re getting answers—plus red flags that mean you should contact a vet urgently.
Índice
Quick Answer
Chronic diarrhea in cats usually means loose or watery stool lasting about 3+ weeks (or recurring episodes that keep returning). The most common causes are parásitos, diet intolerance/food allergyy chronic intestinal inflammation (IBD/chronic enteropathy)—but older cats may also need checks for thyroid, kidney, or cancer-related disease. If it’s ongoing, plan a vet visit and bring a fresh stool sample; seek urgent care if your cat has blood, dehydration, repeated vomiting, severe lethargy, or rapid weight loss.
Principales conclusiones
- Definition: Chronic diarrhea is stool that stays loose/watery for ~3 weeks or longer (or keeps recurring).
- Pattern clue: Large volume + weight loss often points to small bowel; frequent small stools + mucus/straining often points to large bowel/colitis.
- Most common causes: Parasites, diet intolerancey IBD/chronic inflammation are common starting points for investigation.
- Diagnosis is stepwise: Vets often start with stool testing, then bloodwork, then imagingcon un prueba de dieta if food sensitivity is suspected.
- Treatment is cause-specific: The best plan depends on the diagnosis (deworming, prescription diets, probiotics/B12, anti-inflammatory meds, etc.).
- Home care supports recovery: Focus on hydration, diet consistency, and vet-approved probiotics/fiber; avoid human anti-diarrheals unless a veterinarian directs you.
When to call a vet urgently (red flags)
If your cat has diarrhea plus any of the following, don’t wait—contact your vet the same day (or an emergency clinic if severe):
Go to urgent/emergency care now if:
- Diarrhea is very watery/abundant and your cat seems weak, collapsed, or unable to stay alert
- Stool is black/tarry (possible digested blood)
- Diarrhea comes with repeated vomiting, or your cat can’t keep water down
- Signs of deshidratación: sticky/tacky gums, sunken eyes, marked weakness
- Your cat shows significant pain (hunched posture, crying, won’t be touched)
Call your vet today if:
- Your cat is not eating, lethargic, or “just not themselves”
- You see blood or lots of mucus in the stool (especially if increasing)
- Your cat is a kitten, senior, or has another health condition (kidney disease, diabetes, etc.)
- Diarrhea persists beyond 1–2 days or is getting worse
(When in doubt, calling your vet is the safest move.)
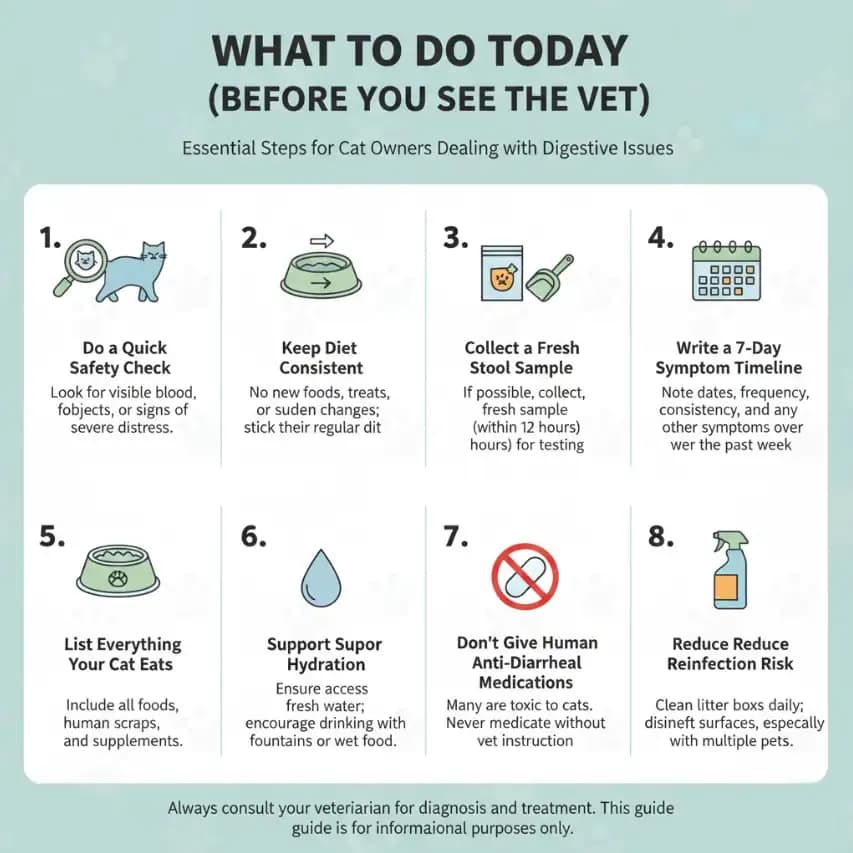
What to Do Today (Before You See the Vet)
If your cat’s diarrhea has lasted 3+ weeks, use this checklist to stay safe and collect the right info for your veterinarian.
1. Do a quick safety check
- If you see a lot of blood, black/tarry stool, repeated vomiting, severe lethargy, or signs of dehydration, seek urgent care.
2. Keep diet consistent (don’t experiment randomly)
- Feed your cat their current diet on schedule unless your vet tells you to start a trial.
- Avoid sudden switches, rich treats, dairy, and “new” foods that make it harder to identify the real trigger.
3. Collect a fresh stool sample
- Save a small amount (about a teaspoon) in a clean bag/container.
- If you can’t go to the vet immediately, refrigerate it and bring it as soon as possible (don’t freeze unless your clinic instructs you).
4. Write a 7-day symptom timeline
- When it started, how often your cat poops, any vomiting, appetite/energy changes, and weight change if you know it.
- Note whether it looks more like:
- Large-volume watery stools (often “small-bowel” pattern), or
- Small frequent stools with mucus/straining (often “large-bowel” pattern)
5. List everything your cat eats (including “small” extras)
- Food brand/flavor, treats, human food, flavored supplements, new chews, lickable treats, etc.
- Include any new medications started in the last month.
6. Support hydration
- Offer fresh water and consider switching to comida húmeda if your cat tolerates it.
- If your cat won’t drink, call your vet—hydration matters more than “stopping diarrhea” in the short term.
7. Don’t give human anti-diarrheal medications
- Avoid Imodium, Pepto-Bismol, Kaopectate, etc. unless a veterinarian explicitly directs you.
8. Reduce reinfection risk (especially if parasites are possible)
- Scoop the litter box promptly, clean soiled areas, and wash bedding.
- If you have multiple cats, ask your vet whether you should separate boxes temporarily.
Take a photo of the stool (gross, but vets genuinely use it), and bring your notes + sample to the appointment.
¿Qué es la diarrea crónica en los gatos?
Diarrea crónica en gatos means loose, soft, or watery stools that persist for about 3 weeks or longer (or keep recurring in repeated episodes). It’s a symptom, not a disease, which usually signals an underlying digestive issue—or less commonly, a whole-body condition.
Key clarifications:
- Why it happens: stool moves through the intestines too quickly (or the gut can’t absorb water/nutrients properly), leading to loose stool.
- Por qué es importante: ongoing diarrhea can cause dehydration, weight loss, and nutrient/vitamin deficiencies, especially in kittens and seniors.
- What to track: duration, frequency, stool volume, straining, mucus/blood, appetite, vomiting, and weight change.
Next, use your cat’s stool pattern to tell whether this looks more like small-bowel o large-bowel diarrhea.

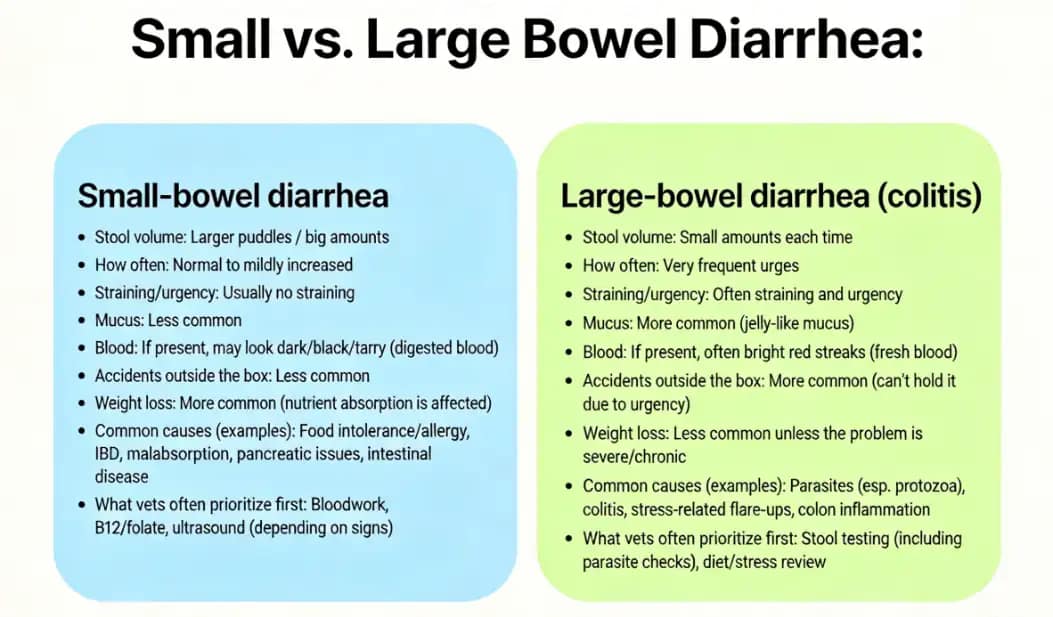
Small vs. Large Bowel Diarrhea: Quick Comparison
Vets often categorize diarrhea by whether it most likely comes from the small intestine or the large intestine (colon). You can’t diagnose the cause at home, but this pattern helps you describe what’s happening clearly—and helps your vet prioritize the right tests.
| Clue you can observe | More consistent with Small-bowel diarrhea | More consistent with Large-bowel diarrhea (colitis) |
|---|---|---|
| Stool volume | Larger puddles / big amounts | Small amounts each time |
| How often | Normal to mildly increased | Very frequent urges |
| Straining/urgency | Usually no straining | Often colar and urgency |
| Mucus | Less common | More common (jelly-like mucus) |
| Blood | If present, may look dark/black/tarry (digested blood) | If present, often bright red streaks (fresh blood) |
| Accidents outside the box | Less common | More common (can’t hold it due to urgency) |
| Weight loss | More common (nutrient absorption is affected) | Less common unless the problem is severe/chronic |
| Common causes (examples) | Food intolerance/allergy, IBD, malabsorption, pancreatic issues, intestinal disease | Parasites (esp. protozoa), colitis, stress-related flare-ups, colon inflammation |
| What vets often prioritize first | Bloodwork, B12/folate, ultrasound (depending on signs) | Stool testing (including parasite checks), diet/stress review |
Mini interpretation guide (what this usually means)
- If you’re seeing large-volume watery stool y pérdida de peso, it leans toward a small-bowel pattern → your vet may recommend broader testing sooner.
- If you’re seeing frequent tiny stools, mucusy straining/urgency, it leans toward a large-bowel/colitis pattern → stool tests and parasite checks often move to the front of the line.
- If you’re seeing a mix of both, that’s common—many cats don’t fit neatly into one category.
Important safety note: Any diarrhea with significant blood, black/tarry stool, repeated vomiting, deshidratacióno letargo warrants prompt veterinary guidance.
Vet Diagnostic Roadmap: How Vets Find the Cause of Chronic Diarrhea
Chronic diarrhea is a síntoma, so the goal is to identify what’s driving it—parasites, diet intolerance, inflammation (IBD), infection/imbalance, endocrine disease, or (less commonly) cancer. Most vets use a stepwise workup, starting with the highest-yield, least invasive steps first.
Step 0: Triage — decide if this is urgent
Your vet may recommend same-day care if there’s deshidratación, repeated vomiting, significant blood, weakness, rapid weight loss, or if your cat is a kitten, senior, diabetic, kidney patient, or immunocompromised.
Step 1: History + exam (this often narrows the list a lot)
Expect questions like:
- How long has it been going on? Constant vs on-and-off?
- Stool pattern: large volume vs small frequent, straining, mucus, blood
- Diet details (brand/flavor), new treats, human foods, food changes
- Indoor/outdoor, shelter history, multi-cat household
- Medications/supplements, recent antibiotics, stress changes
- Weight loss, vomiting, appetite changes, thirst/urination changes
Why this matters: these clues often point toward large-bowel colitis, food intolerance, parásitoso systemic disease before testing even starts.
Step 2: Stool testing (often the first “must-do”)
This step aims to rule out common infectious causes—especially parasites that can be easy to miss.
Common options include:
- Fecal float/smear (screens for worm eggs, some protozoa)
- Giardia testing (antigen tests or PCR depending on clinic)
- PCR panels (can detect organisms like Tritrichomonas foetus and others)
Importante: one negative stool test doesn’t always rule parasites out. Some vets repeat testing or treat empirically if suspicion is high.
Step 3: “Rule-out” deworming or parasite treatment (common even with negative tests)
Because parasites are common and tests aren’t perfect, vets often prescribe a broad dewormer or a targeted anti-parasitic when the history fits (young cat, shelter, multi-cat, intermittent diarrhea, mucus).
Step 4: Basic labwork (especially important in adult/senior cats)
If diarrhea is chronic or your cat is older, vets often add:
- CBC/chemistry (checks anemia, inflammation, protein levels, kidney/liver markers)
- Thyroid test (hyperthyroidism is a classic diarrhea + weight loss cause in older cats)
- Urinalysis (adds context for kidney/metabolic issues)
This step helps differentiate intestinal-only problems from whole-body conditions that can drive diarrhea.
Step 5: Gut-supportive labs (when chronic diarrhea persists)
Depending on your cat’s signs, your vet may recommend:
- Vitamin B12 (cobalamin) level (low B12 is common in chronic enteropathy)
- Folate (helps interpret small intestinal absorption issues)
- Pancreatic markers (if pancreatitis/triaditis is suspected)
These tests can guide treatment even before advanced imaging.
Step 6: Diet trial (a high-yield step that’s often done early)
If parasites/infection aren’t obvious, many vets recommend a strict food trial:
- Hydrolyzed o novel protein diet
- Normalmente 8-12 semanas
- No treats, flavored meds, or table foods during the trial (this is what makes it diagnostic)
If diarrhea improves significantly, that strongly suggests food intolerance/allergy or diet-responsive inflammatory disease.
Step 7: Imaging (when symptoms persist, worsen, or red flags appear)
If the diarrhea continues despite the steps above—or if there’s weight loss, pain, abnormal labs, or vomiting—vets often use:
- X-rays (useful for obstruction patterns or some masses)
- Ultrasound (useful for bowel wall changes, lymph nodes, pancreas/liver involvement)
This step helps rule out structural disease (masses, thickening, partial obstruction) and guides next steps.
Step 8: Advanced testing (for difficult or high-stakes cases)
If chronic diarrhea doesn’t respond to earlier steps, or if the vet needs to distinguish conditions like IBD vs intestinal lymphoma, they may recommend:
- Endoscopy with biopsies (less invasive than surgery, samples lining)
- Surgical biopsies (deeper samples if needed)
- Referral to internal medicine (often worth it for persistent weight loss or unclear imaging)
What you can bring to make the workup faster
- A fresh stool sample (small amount is enough)
- A 7-day note of stool consistency + frequency + vomiting
- Food labels/photos + list of treats/supplements/meds
- Photos of stool if it changes day to day
Common Causes of Chronic Diarrhea in Cats (Most Likely First)
Chronic diarrhea can have many causes, but most cats end up in a few common, treatable buckets. Vets typically prioritize based on:
- Stool pattern: small-bowel vs large-bowel clues
- Age: kittens vs seniors have different “top suspects”
- Exposure risk: outdoors, shelter history, multi-cat homes
- Otros signos: weight loss, vomiting, appetite changes, lethargy
Below are the most common causes in the order they’re often ruled out—with quick clues to help you and your vet narrow it down.
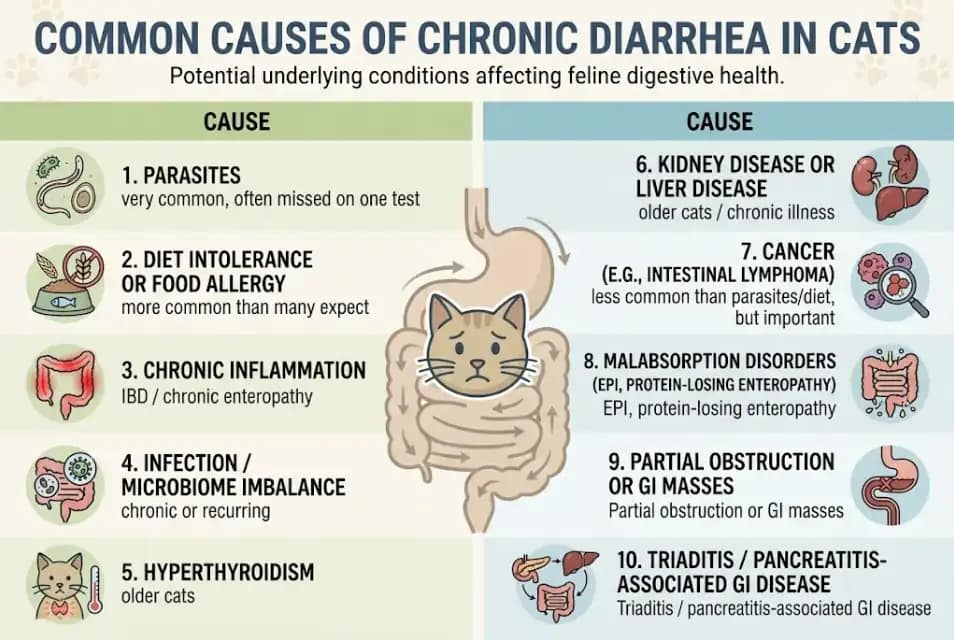
1. Parasites (very common, often missed on one test)
- Most likely if: kitten/young cat, shelter/cattery background, multi-cat home, foul-smelling stool, mucus, intermittent diarrhea.
- Vet often checks: fecal float + antigen/PCR tests; sometimes treats empirically if suspicion is high.
- Safe now: bring a fresh stool sample; clean litter boxes daily; isolate affected cats if possible.
Los parásitos intestinales son una de las principales causas de heces blandas crónicas, sobre todo en gatos jóvenes o procedentes de refugios/gaterías. Protozoos como Giardia y Tritrichomonas foetusLas lombrices, o gusanos comunes (ascárides, anquilostomas, tricocéfalos), pueden vivir en el intestino y causar diarrea persistente.
Por ejemplo, Tritrichomonas foetus es un protozoo que a menudo causa diarrea crónica de intestino grueso con mucosidad en gatos jóvenes - un estudio del Reino Unido lo encontró en alrededor del 14% de los gatos diarreicos, sobre todo en gatitos con pedigrí.
Giardia es otro parásito molesto que puede causar diarrea maloliente e intermitente. Aunque hayas desparasitado a tu gato, algunos parásitos requieren pruebas específicas para detectarlos.
2. Diet intolerance or food allergy (more common than many expect)
- Most likely if: diarrhea started after a food/treat change, recurrent episodes, mild vomiting, itchy skin/ear issues, otherwise “mostly normal” cat.
- Vet often checks: strict diet history, then a prescription diet trial (hydrolyzed or novel protein).
- Safe now: don’t keep switching foods rapidly; write down everything the cat eats (including treats/flavored meds).
La diarrea relacionada con la comida es más frecuente de lo que muchos propietarios de gatos creen. Los gatos pueden desarrollar una alergia a una proteína (por ejemplo, pollo o ternera) o una intolerancia a determinados ingredientes. El resultado puede ser una diarrea crónica, a veces con vómitos o picor en la piel.
De hecho, la investigación ha demostrado que alrededor de 30% de los gatos con diarrea crónica idiopática resultan tener sensibilidad alimentaria y mejorar con una dieta hipoalergénica.
Por eso los veterinarios suelen sugerir un prueba de dieta al principio del proceso: no es invasivo y puede ser muy gratificante si la diarrea se resuelve con un simple cambio de alimentación.
3. Chronic inflammation (IBD / chronic enteropathy)
- Most likely if: long-term on-and-off diarrhea, vomiting, weight loss, poor appetite periods, B12 deficiency, multiple recurrences.
- Vet often checks: bloodwork, B12, ultrasound; sometimes biopsy if severe or not responding.
- Safe now: keep a symptom log; don’t use human antidiarrheals; follow vet diet/med plan consistently.
Some intestinal cancers can look similar to IBD, so persistent weight loss or poor response to treatment may prompt imaging or biopsy.
La EII es una diagnóstico común de la diarrea crónica en gatos. Es una enfermedad en la que el revestimiento intestinal está infiltrado por células inflamatorias (algo así como el SII felino, pero con inflamación real).
Cats with IBD often have intermittent vomiting and diarrhea, weight loss, and abnormal stool that can be small or large bowel in nature. IBD is essentially an overactive immune response in the gut – triggers could be certain foods or bacterial imbalances.
A menudo es necesaria una biopsia para diagnosticarla definitivamente. Muchos gatos con EII responden a cambios en la dieta (nuevas dietas proteicas) o a medicamentos como los corticosteroides para reducir la inflamación.
4. Infection / microbiome imbalance (chronic or recurring)
- Most likely if: stress event + diarrhea, post-antibiotics diarrhea, multi-cat homes, intermittent flare-ups, mucus/colitis patterns.
- Vet often checks: fecal tests, sometimes targeted treatment + probiotics.
- Safe now: avoid unnecessary antibiotics; use vet-recommended probiotics if advised.
Ciertas bacterias y virus pueden provocar diarreas continuas. Dos bacterias infames son Clostridium perfringens y Campylobacter - pueden alterar la flora intestinal, especialmente después de estrés o uso de antibióticos.
Crónica infecciones víricas como el virus de la leucemia felina (FeLV) o el virus de la inmunodeficiencia felina (FIV) también pueden causar diarrea o hacer que un gato sea más propenso a infecciones secundarias.
Por lo general, las infecciones también provocan otros signos (fiebre, falta de apetito), pero las infecciones crónicas leves pueden presentarse principalmente como heces blandas.
In kittens and young cats, prioritize these early
- Giardia (often intermittent, smelly diarrhea)
- Tritrichomonas foetus (often chronic large-bowel diarrhea with mucus in young cats)
- Roundworms/hookworms (common and treatable)
5. Hyperthyroidism (older cats)
- Most likely if: senior cat, weight loss + ravenous appetite, hyperactivity, increased thirst, vomiting sometimes.
- Vet often checks: T4 thyroid test.
- Safe now: schedule bloodwork; don’t assume it’s “just food.”
Los gatos con una tiroides hiperactiva suelen tener el metabolismo acelerado. Junto con la pérdida de peso y la hiperactividad, pueden padecer diarrea crónica porque el exceso de hormona tiroidea acelera el tránsito intestinal.
Si su gato es de mediana edad o mayor y tiene diarrea además de apetito voraz y pérdida de peso, hipertiroidismo es una regla superior.
Un simple análisis de sangre para medir los niveles de tiroides (T4) puede diagnosticarlo, y el tratamiento (medicación u otras terapias) suele resolver la diarrea.
6. Kidney disease or liver disease (older cats / chronic illness)
- Most likely if: older cat, appetite changes, vomiting, increased thirst/urination, weight loss.
- Vet often checks: bloodwork + urinalysis; sometimes ultrasound.
- Safe now: hydration focus, prompt vet follow-up.
La insuficiencia renal avanzada puede causar signos gastrointestinales, como diarrea o vómitos. La uremia (niveles elevados de toxinas por insuficiencia renal) irrita la mucosa gastrointestinal.
Además, algunas dietas o suplementos renales pueden no sentar bien en el estómago de todos los gatos, provocando heces más blandas.
Si su gato tiene problemas renales conocidos y desarrolla heces blandas crónicas, puede estar relacionado; el tratamiento de la enfermedad renal y el uso de protectores intestinales suelen ayudar.
In addition. The liver produces bile acids that aid digestion. Liver dysfunction or bile duct issues can lead to maldigestion and diarrhea.
Por ejemplo, los gatos con colangiohepatitis o tumores hepáticos pueden presentar diarrea intermitente, a menudo junto con otros signos como ictericia o inapetencia.
7. Cancer (e.g., intestinal lymphoma) — less common than parasites/diet, but important
- Most likely if: progressive weight loss, appetite drop, poor response to diet trials/parasite treatment, abnormal imaging/bloodwork.
- Vet often checks: ultrasound, biopsy/endoscopy if indicated.
- Safe now: don’t delay if weight loss is ongoing.
Los cánceres pueden causar diarrea tanto si están en el tracto GI como en otros lugares. El cáncer GI más común en gatos es linfoma alimentario (un tipo de cáncer intestinal), que puede parecerse a la EII: diarrea crónica del intestino delgado y pérdida de peso.
El linfoma suele necesitar quimioterapia o esteroides. Otros cánceres fuera del GI (como los tumores de mastocitos o el cáncer generalizado) pueden liberar sustancias o provocar respuestas al estrés que también provocan diarrea.
Si la diarrea crónica de un gato se debe a un cáncer, a menudo otros signos (como una pérdida grave de peso o cambios en los análisis de sangre) apuntarán en esa dirección.
8. Malabsorption disorders (EPI, protein-losing enteropathy)
- Most likely if: greasy/voluminous stool, major weight loss despite eating, low protein/B12.
- Vet often checks: specialized blood tests, B12, ultrasound.
- Safe now: prompt vet workup; don’t rely on home remedies alone.
Si un gato no puede digerir o absorber correctamente los nutrientes, puede sufrir diarrea. Un ejemplo clave es Insuficiencia pancreática exocrina (IPE) - una enfermedad poco frecuente en los gatos en la que el páncreas no produce suficientes enzimas digestivas.
Los gatos con EPI tienen diarrea voluminosa y grasa y pérdida de peso a pesar de tener buen apetito. Otro ejemplo es enteropatía perdedora de proteínasEn el caso de enfermedades como la EII, el intestino pierde proteínas, lo que a menudo provoca diarrea crónica y pérdida de peso.
Estas afecciones suelen aparecer en los análisis de sangre (como niveles bajos de B12 o de proteínas).
9. Partial obstruction or GI masses
- Most likely if: alternating diarrhea/constipation, vomiting, belly discomfort, poor appetite, foreign-object risk.
- Vet often checks: X-ray/ultrasound.
- Safe now: urgent vet visit if vomiting/lethargy occurs.
A veces, una obstrucción parcial en los intestinos (por ejemplo, por la ingestión de un objeto extraño, o un pólipo/tumor en el intestino) puede causar diarrea intermitente. La obstrucción puede permitir el paso de algunas heces, pero irrita el intestino o provoca una mala digestión parcial.
Cats with an obstruction might have alternating diarrhea and constipation, or vomiting as well. This is where imaging (X-ray or ultrasound) becomes important to rule out any physical blockage.
10. Triaditis / pancreatitis-associated GI disease
- Most likely if: vomiting + poor appetite + diarrhea, recurring flares, ultrasound findings, B12 issues.
- Vet often checks: bloodwork, ultrasound, pancreatic/liver markers, B12.
- Safe now: follow vet diet/med plan; consistency matters.
Los gatos tienen una tendencia única a desarrollar una inflamación combinada del intestino, el hígado y el páncreas, una tríada de problemas conocida (convenientemente) como triaditis. La diarrea crónica en gatos con triaditis suele ir acompañada de vómitos y falta de apetito.
Essentially, it’s IBD + pancreatitis + cholangitis (bile duct inflammation) occurring together. Managing triaditis often requires a multifaceted approach (diet change, B12 shots, anti-inflammatory meds, etc.), but recognizing it explains why some cats have so many GI symptoms at once.
No se trata de una lista exhaustiva (otras causas poco frecuentes son las infecciones fúngicas, FIP que provocan lesiones intestinales granulomatosas, etc.), pero éstos son los más importantes. La buena noticia: muchas de estas las causas intestinales pueden tratarse o gestionarse una vez identificados.
Most cats with chronic diarrhea fall into the “common bucket” (parasites, diet intolerance, inflammation). The goal is to rule out the easy, treatable causes first, then escalate testing if the diarrhea persists or your cat is losing weight or acting unwell.

Opciones de tratamiento de la diarrea del gato
Chronic diarrhea has two parallel goals:
- Make your cat stable and comfortable (firm stool, prevent dehydration, protect the gut).
- Treat the underlying cause (parasites, diet intolerance, IBD, thyroid/kidney disease, etc.) so diarrhea doesn’t keep returning.
What changes stool fastest vs what treats the cause
Here’s the key idea: some steps can improve stool within days, but they may not “cure” the problem unless the root cause is addressed.
| Goal | What often helps fastest | Typical time to notice change | What it doesn’t solve |
|---|---|---|---|
| Stabilize stool / reduce urgency | Diet consistency, vet-approved probiotics, hydration support, fiber if large-bowel pattern | 24–72 hours (sometimes longer) | Won’t fix parasites, endocrine disease, tumors |
| Treat the cause | Deworming/anti-parasitics, strict diet trial, anti-inflammatory meds (IBD), thyroid/kidney management | Days → weeks (diet trials often 8-12 semanas) | May not “look better” immediately |
*Every cat is different. If you see blood, dehydration, repeated vomiting, severe lethargy, or rapid weight loss, don’t wait—contact a veterinarian urgently.
A practical timeline (so you know what “working” looks like)
- Within 24–72 hours: you’re looking for stool to move from watery → pudding-like → soft-formed, and for your cat to stay hydrated and bright.
- Within 1–2 weeks: you should see a clear trend if a parasite plan or supportive plan is correct.
- Within 8–12 weeks (diet trial): this is when food intolerance/IBD diet response becomes convincing—only if the trial is strict (no treats, flavored meds, or food extras).
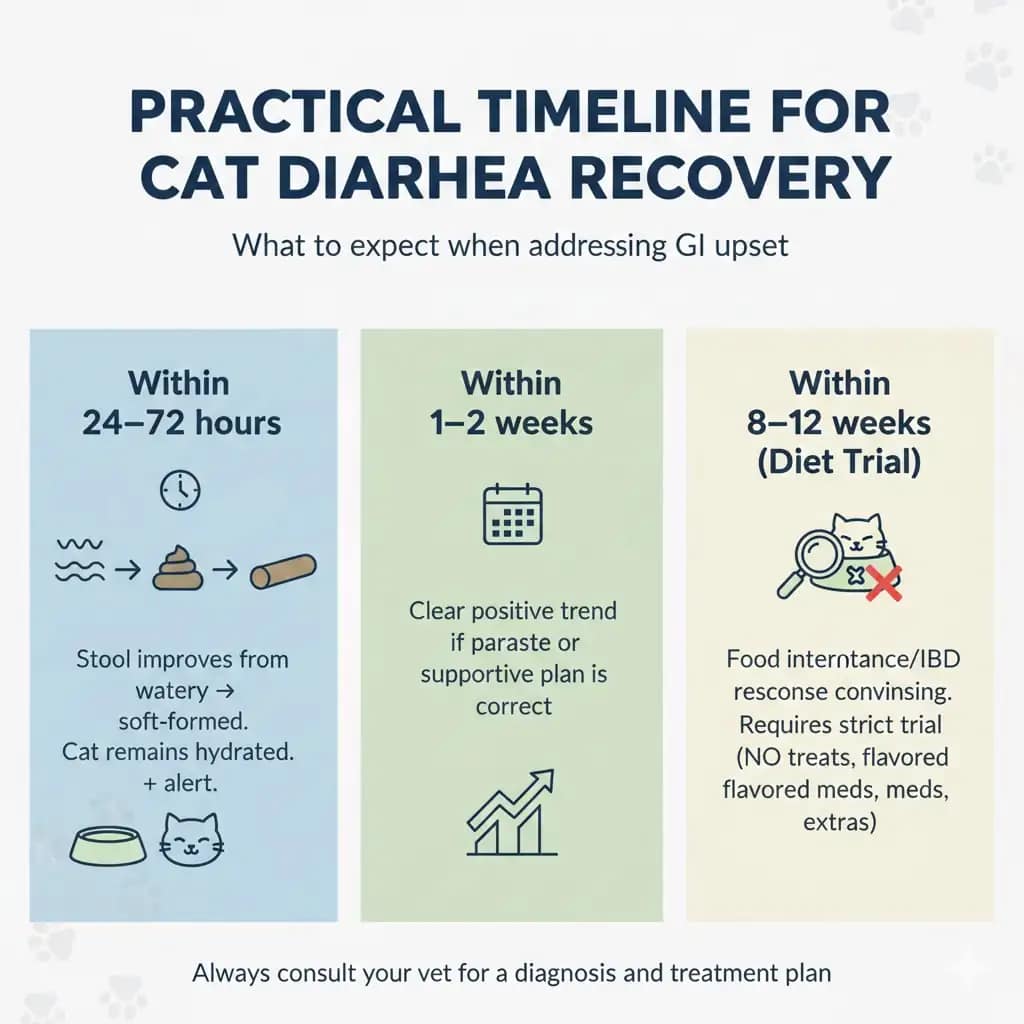
Si su gato tiene blood, dehydration, repeated vomiting, lethargy, or rapid weight loss, skip the “wait and see” window and contact a vet urgently.
Si te sientes abrumado o quieres más orientación paso a paso adaptada específicamente a los padres de gatos, tenemos todo lo que necesitas. Echa un vistazo a nuestra guía práctica y detallada, diseñada especialmente para los propietarios de gatos: Tratamiento de la Diarrea del Gato: Guía para padres de gatos
The main treatment strategies by category
Desparasitación y antiparasitarios
If tests show (or strongly suspect) parasites, your veterinarian will prescribe medication to eliminate them. Common options may include fenbendazol (used for Giardia and some worms) and praziquantel (tapeworms). For Tritrichomonas foetus, veterinarians may use a specific prescription medication such as ronidazol.
Because parasites can be hard to fully rule out (shedding can be intermittent), vets sometimes recommend empirical deworming even if an initial fecal test is negative—especially in kittens, shelter cats, or multi-cat homes.
- When it’s used: parasite risk is high, stool tests suggest parasites, or the diarrhea pattern fits common parasite causes.
- What improvement looks like + timing: if parasites are the main driver, stool often improves within 3–7 days, sometimes up to 1–2 weeks depending on the organism and treatment plan.
- If there’s no improvement: ask your vet about repeat stool testing / PCR (including Giardia/Tritrichomonas where relevant) and whether the next step should be a prueba de dieta or broader workup.
Terapia dietética
Diet changes are a cornerstone of chronic diarrhea care—but they’re used in two different ways:
- Diet for faster stool support: gentle digestion and more consistent stool (often days to 1–2 weeks)
- Diet as a root-cause test/treatment: proving and managing food intolerance or IBD (often weeks; a convincing trial is usually 8-12 semanas)
Highly Digestible, Low-Fat/High-Fiber Diet (support-focused)
This approach (often a veterinary GI diet) is designed to be gentle and easy to absorb. Fiber can help regulate stool consistency and can support beneficial gut bacteria.
This may be used for cats with “sensitive stomach,” mild pancreatitis concerns, some infections/imbalances, or chronic diarrhea where a gentle baseline diet is needed while diagnostics are underway.
Unlike dogs, many cats don’t require aggressively low-fat diets unless pancreatitis is a factor—but a highly digestible formula is commonly tried early because it’s easy on the gut.
Novel Protein or Hydrolyzed Protein Diet (cause-focused)
This is often recommended for suspected food intolerance/allergy o IBD.
A novel protein diet uses a protein your cat hasn’t eaten before (e.g., rabbit, duck, venison—availability varies). A hydrolyzed diet uses proteins broken into smaller fragments to reduce immune triggering.
For many cats, a strict trial (no treats, no flavored toppers, no “just a bite” of other foods) for 8-12 semanas can lead to major improvement if food intolerance is the cause. Blood tests for food allergies in cats are not very reliable, so the diet trial is often the most meaningful proof.
If a cat has large-bowel signs (mucus/urgency/straining), your vet may recommend adding a small amount of soluble fiber (like canned pumpkin or psyllium) to an appropriate complete diet—but do this only with guidance so the diet stays balanced.
Any diet change should usually be introduced gradually over 7–10 days unless your veterinarian instructs otherwise.
- When it’s used: as early supportive care, and/or as a diagnostic tool for food intolerance/IBD.
- What improvement looks like + timing: consistency alone may improve stool within 3–7 days, but a true food-response usually becomes clear over weeks—and a valid trial is typically 8-12 semanas.
- If there’s no improvement: avoid switching foods repeatedly. Confirm the trial was truly strict, then ask your vet whether to change diet type (novel vs hydrolyzed) or escalate testing (bloodwork/imaging/IBD evaluation).
Probióticos y suplementos intestinales
Probiotics may help some cats with chronic diarrhea by supporting a healthier gut microbiome. Vets often recommend feline-specific probiotic powders or pastes that can be mixed into food.
Think of probiotics as stool-support helpers, not a standalone cure—especially if the underlying cause is parasites, endocrine disease, or chronic inflammation.
Another supplement that may be needed is vitamina B₁₂ (cobalamina). Cats with chronic enteropathy can have low B₁₂, which may worsen appetite and GI function. Veterinarians may recommend injections or high-dose oral B₁₂ depending on the case.
- When it’s used: alongside diagnostics, during diet trials, after antibiotics, or with chronic enteropathy/IBD plans.
- What improvement looks like + timing: some cats show stool improvement in 3–7 days, others take 2-4 semanas. B₁₂ support often helps energy/appetite over weeks.
- If there’s no improvement: review whether the root cause is being treated (parasites/diet/IBD/systemic disease) and ask your vet if further testing is needed.
Cuidados de apoyo
Never give human anti-diarrheal medications to cats unless your veterinarian explicitly instructs you. Products like Imodium (loperamide) o Pepto-Bismol can be dangerous for cats, and slowing the gut can be risky if an underlying condition needs urgent care.
With chronic diarrhea—especially if severe—supportive care may be needed to prevent dehydration and keep your cat comfortable. Fluidoterapia may be recommended if your cat is dehydrated (sometimes subcutaneous fluids are used under veterinary direction).
Vets may occasionally prescribe medications to support the gut (for example, protectants or targeted therapies), but these are usually adjuncts. The long-term solution is still diet strategy, parasite control, and inflammation/systemic disease management when indicated.
- When it’s used: when dehydration risk is present, stool is very watery/frequent, or comfort support is needed while diagnostics are underway.
- What improvement looks like + timing: hydration support can improve energy quickly; stool typically improves as the trigger is controlled (often days, sometimes longer).
- If there’s no improvement: persistent severe diarrhea despite supportive care is a reason to escalate diagnostics (repeat stool tests, bloodwork, imaging, and possibly specialist evaluation).

Consejos caseros para gatos con diarrea crónica
Dealing with chronic diarrhea isn’t just a veterinary journey—it’s also about daily home management. There’s a lot you can do to keep your cat comfortable and support recovery.
Think of yourself and your vet as a team: your vet provides the medical plan, and you provide consistent support at home to maximize success.
Home care goals (what you’re trying to accomplish)
- Prevent dehydration and keep your cat eating
- Reduce gut irritation by avoiding sudden changes
- Support stool formation with vet-approved diet/probiotics/fiber
- Track symptoms clearly so your vet can diagnose faster
What to do today (quick checklist)
- Keep food consistent (unless your vet has started a diet trial).
- Encourage hydration (fresh water + wet food if appropriate).
- Scoop the litter box more often and consider an extra box nearby.
- Start a simple daily log (template below).
- If your cat seems worse, call your vet—don’t wait it out.
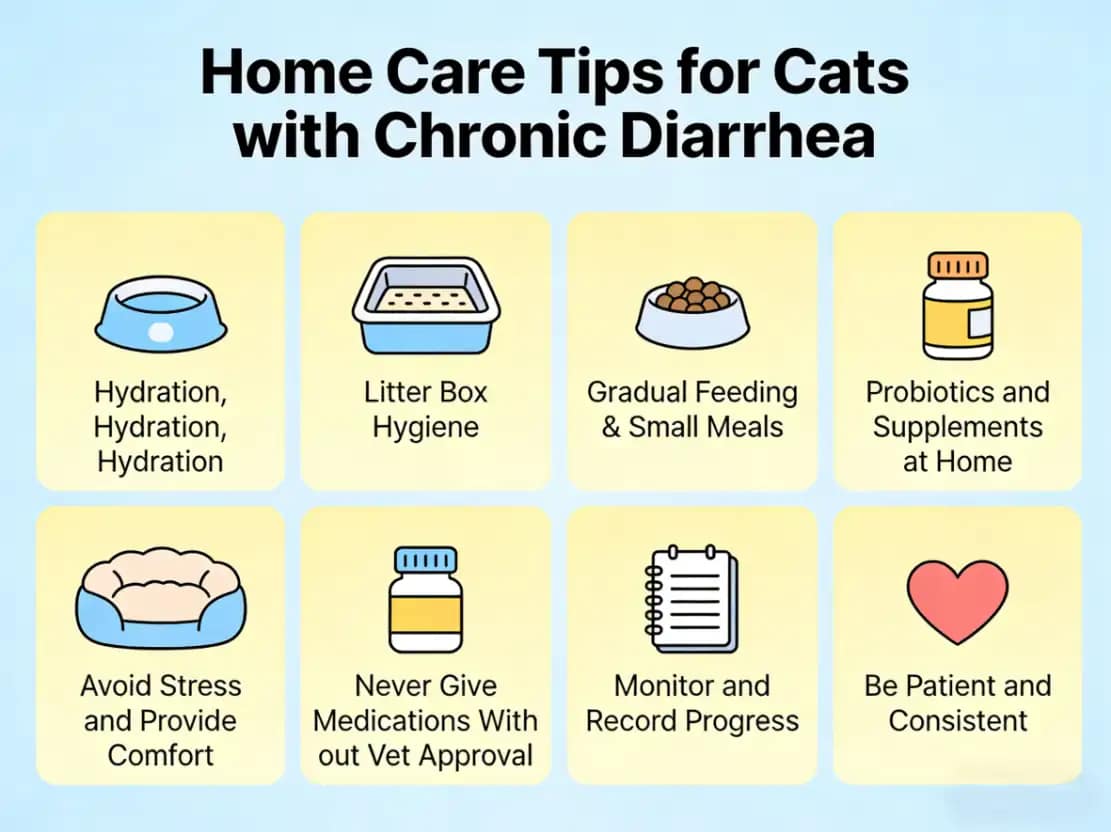
Hidratación, hidratación, hidratación
Qué hacer
- Keep agua dulce available in multiple places.
- Try a cat fountain (many cats drink more from moving water).
- If your vet agrees, offer more moisture-rich meals (wet food or adding a little water to food).
Why it helps
Diarrhea causes fluid and electrolyte loss. Even mild dehydration can worsen appetite, energy, and recovery.
Watch for (call your vet)
Sticky or dry gums, weakness, sunken eyes, or your cat refusing to drink.
Higiene de la caja de arena
Qué hacer
- Scoop frequently and keep the box extra limpio (diarrhea can cause urgency).
- Add an extra litter box closer to where your cat spends time to prevent accidents.
- Utilice unscented, soft litter to reduce irritation.
- If your cat has long hair, consider a sanitary trim to prevent stool sticking.
Why it helps
A clean, easy-to-reach box reduces stress and helps your cat maintain good litter habits—even when they feel urgent.
Watch for
Straining, frequent tiny stools, or accidents outside the box that suddenly worsen (these can signal large-bowel irritation or worsening discomfort).
Alimentación gradual y comidas pequeñas
Qué hacer
- Oferta small, frequent meals instead of one or two large meals.
- Serve food at temperatura ambiente (some cats do better than with cold food).
- Keep the diet steady day-to-day unless your vet has instructed a specific diet trial.
Why it helps
Smaller meals are easier to digest and may reduce intestinal overload.
Avoid
- Sudden food changes
- Too many treats “to tempt appetite” (often makes diarrhea worse)
Probióticos y suplementos en casa
What to do (vet-guided)
- If your vet recommends it, use a probiótico específico para felinos daily.
- If prescribed, give vitamina B₁₂ (cobalamina) as directed (low B₁₂ can worsen gut healing).
- If your vet approves fiber: start very small and increase slowly.
Common vet-approved fiber options
- Plain canned pumpkin (not pie filling)
- Psyllium husk (often used for large-bowel diarrhea)
Why it helps
Probiotics can support healthier gut bacteria, and fiber can help normalize stool consistency in some cats—especially with large-bowel patterns.
Watch for
Gas, worsening stool, or reduced appetite after adding fiber (pause and ask your vet).
Evitar el estrés y proporcionar comodidad
Qué hacer
- Keep routines stable: same feeding time, same litter box location, same sleeping area.
- Provide a quiet resting spot and minimize big environmental changes if possible.
- Offer gentle comfort—snuggles, brushing, calm play—based on what your cat enjoys.
Why it helps
Stress can trigger or worsen diarrhea in sensitive cats, so a calm environment supports gut recovery.
Nunca administre medicamentos sin la aprobación del veterinario
Importante: Visite no give human anti-diarrheal medications unless your vet explicitly instructs you.
That includes Imodium (loperamide), Pepto-Bismol (bismuth subsalicylate), Kaopectate, and similar products.
Cats process drugs differently than humans (and even dogs), and some medications can be unsafe or toxic. If you want to do more than diet + probiotics + hydration, ask your vet about feline-safe options.
Supervisar y registrar los progresos
Tracking symptoms helps you see what’s improving—and gives your vet the exact information needed to adjust the plan.
What to track daily (60 seconds)
- Stool: formed / soft / watery
- Frequency: how many bowel movements
- Add-ons: blood, mucus, straining
- Appetite + energy
- Any vomiting
Template 1: 7-Day Stool & Symptom Log (copy/paste)
| Fecha | Stool (formed/soft/watery) | # BMs | Blood/mucus? | Straining? | Vomiting? | Appetite | Energy | Food/treats | Notas |
|---|
Template 2: Bring-to-the-Vet Checklist (copy/paste)
Bring these to help your vet diagnose chronic diarrhea faster:
- A fresh stool sample (small amount is enough)
- Food label/photo: exact brand + flavor, treats, toppers
- List of medications, supplements, flea/tick products
- En 7-day log (above)
- Any recent changes: new pet, boarding, moving, stress events
- Photos of stool (gross, but genuinely helpful)
- Weight changes you’ve noticed
Be Patient and Consistent
Chronic conditions improve gradually—overnight fixes are uncommon. Follow your vet’s plan closely:
- Finish prescribed medications even if stool improves early.
- Keep the diet strict during trials (no treats unless approved).
- Give changes time to work—diet trials often take weeks, not days.
When home care isn’t enough (call your vet promptly)
Contact your vet if:
- Diarrhea persists despite steady home care for 3–5 days
- Your cat is losing weight
- You see sangre, black/tarry stool, or significant mucus
- There’s vomiting, refusal to eat, or obvious abdominal pain
- Your cat is a kitten, senior, or has chronic illness (kidney disease, diabetes, etc.)

Conclusión
Chronic diarrhea in cats—loose or watery stools that last 3+ weeks or keep coming back—is a síntoma, not a diagnosis. The most common underlying causes include parásitos, diet intolerance/food allergyy chronic intestinal inflammation (IBD/chronic enteropathy), though older cats may also need screening for thyroid, kidney, or intestinal disease.
The fastest way to get answers is a step-by-step plan with your veterinarian: track stool changes, bring a fresh stool sample, and follow the recommended workup (often stool testing, basic bloodwork, and sometimes a structured diet trial). While you’re sorting out the cause, focus on hydration, diet consistencyy vet-approved supportive options like probiotics or fiber—never human anti-diarrheal medications unless your vet specifically directs it.
Most importantly, don’t wait if you notice blood in the stool, repeated vomiting, dehydration, severe lethargy, rapid weight loss, or if your cat is a kitten or senior. With timely veterinary care and consistent home support, many cats can return to comfortable, healthy bathroom habits.
If you’re feeling overwhelmed, you’re not alone. Your veterinarian is your best partner—and many cat parent communities can help you feel supported while you work through the process.
¿Necesita más ayuda?
Want a complete, practical hub on feline diarrhea—symptoms, urgent warning signs, vet testing, safe home care, and prevention?
Read next: Diarrea del gato: Todo lo que debe saber
En SnuggleSoulsLa misión de nuestro equipo es ayudarte a resolver estos problemas de la vida real, no sólo darte información de manual. Estamos aquí para ti y para los miembros de tu familia felina en cada paso del camino.
PREGUNTAS FRECUENTES
¿Cómo puedo saber si la diarrea de mi gato es crónica?
Diarrhea is usually considered chronic when loose or watery stools last 3 weeks or longer, or keep returning in repeated episodes. Chronic diarrhea suggests an underlying issue (like parasites, diet intolerance, or intestinal inflammation) rather than a one-time upset stomach. If it has lasted more than a few days—or your cat is a kitten, senior, or losing weight—schedule a vet visit.
¿Cuáles son las causas más frecuentes de diarrea crónica en los gatos?
Las causas más frecuentes son parásitos (especially in young cats), diet intolerance/food allergy, chronic intestinal inflammation (IBD/chronic enteropathy)y infection or gut microbiome imbalance. In older cats, vets also commonly check for hipertiroidismo, enfermedad renaly a veces intestinal cancer. Stool pattern (small-bowel vs large-bowel) plus basic tests usually narrows this quickly.
¿Cuándo debo llevar a mi gato al veterinario por diarrea?
Go to the vet the same day if there’s sangre, repeated vomiting, marked lethargy, dehydration, belly pain, or your cat can’t keep water down. If your cat otherwise seems okay but diarrhea lasts more than 48–72 hours, or keeps recurring, book an appointment. If diarrhea reaches the 3-week mark, it’s chronic and should be evaluated.
¿Puedo darle a mi gato medicación humana para la diarrea?
No—don’t give human anti-diarrheal medicines unless your veterinarian specifically tells you to. Some products (including common options like loperamide/Imodium or bismuth/Pepto-Bismol) can be unsafe for cats or can mask symptoms while the real cause worsens. Ask your vet for cat-safe options instead.
¿Qué alimentos ayudan a detener la diarrea crónica en los gatos?
There isn’t one “best food” for every cat—diet choice depends on the cause. Vets commonly use a strict diet trial con un hydrolyzed o novel-protein diet for 8-12 semanas when food intolerance/IBD is suspected, or a highly digestible GI diet when the gut needs rest. Avoid frequent food switching; change diets only with a plan, and keep treats/flavored add-ons out during a trial.
¿Ayudan realmente los probióticos a los gatos con diarrea crónica?
Probióticos puede ayudar some cats by supporting a healthier gut bacterial balance, especially alongside diet management. Choose a cat-specific product and give it consistently for 1–2 weeks to judge response. If diarrhea worsens, your cat refuses food, or there are red flags (blood, vomiting, lethargy), stop and contact your veterinarian—probiotics don’t replace diagnosis.
¿Es grave la diarrea crónica en los gatos?
Yes—ongoing diarrhea can cause dehydration, weight loss, and nutrient deficiencies, and it can signal problems like parasites, chronic inflammation, endocrine disease, or more serious illness in older cats. If diarrhea is persistent or recurring, the safest approach is a vet workup (often starting with stool testing and basic bloodwork) so the underlying cause can be treated.
¿Cuánto tiempo se tarda en curar la diarrea crónica en los gatos?
The timeline depends on the cause. Parasite-related diarrhea may improve within days to 1–2 weeks after correct treatment, while diet-related cases often require several weeks (and a full 8–12 week diet trial) to confirm improvement. Conditions like IBD may need long-term management. If there’s no improvement within 1–2 weeks of a vet-guided plan, follow up.
¿Puede el estrés causar diarrea crónica en los gatos?
Estrés can trigger or worsen diarrhea in sensitive cats, especially large-bowel/colitis-type symptoms. However, diarrhea that persists beyond a few days—or keeps returning—shouldn’t be assumed to be “just stress,” because parasites, diet intolerance, and inflammation are also common. Reduce stressors, keep diet consistent, and involve your vet if symptoms continue.
Referencias
Tricounty Animal Hospital. (s.f.). Diarrea crónica en gatos - Visión general. Obtenido de https://tricountyah.com/pet-health/chronic-diarrhea-cats/
Veterinaria Puerta Pequeña. (s.f.). Diarrea en gatos. Obtenido de https://www.smalldoorvet.com/learning-center/medical/diarrhea-in-cats/
Hospitales VCA. (s.f.). Pruebas de diarrea. Obtenido de https://vcahospitals.com/know-your-pet/testing-for-diarrhea
Marks, S. L. (2020). Vómitos. En Medicina interna de pequeños animales (6ª ed.). Elsevier. Obtenido de https://pmc.ncbi.nlm.nih.gov/articles/PMC7161394/
Laflamme, D. P., & Xu, H. (2024). Dietary management of feline diarrhea: A review of the evidence. Revista de medicina y cirugía felinas, 12(1), 44. Obtenido de https://pmc.ncbi.nlm.nih.gov/articles/PMC11104099/
PetMD. (2024, 9 de abril). Gato Diarrhea Treatment. Obtenido de https://www.petmd.com/cat/general-health/cat-diarrhea-treatment
LolaHemp. (2025, 5 de marzo). Cat Diarrhea Home Remedy. Obtenido de https://lolahemp.com/blogs/cat-health/cat-diarrhea-home-remedy
Hospitales VCA. (s.f.). 8 remedios caseros para la diarrea y 2 que son peligrosos para tu mascota. Obtenido de https://vcahospitals.com/shop/articles/8-home-remedies-for-diarrhea-and-2-that-are-dangerous-for-your-pet
Tams, T. R. (2011, 1 de octubre). Tratamiento de la EII y la diarrea en gatos adultos. DVM360. Obtenido de https://www.dvm360.com/view/managing-ibd-and-diarrhea-adult-cats-proceedings
Socios veterinarios de BluePearl. (2020, 21 de septiembre). Chequeo intestinal: Tratamiento práctico de la enfermedad inflamatoria intestinal. Obtenido de https://bluepearlvet.com/medical-library-for-dvms/gut-check-practical-treatment-of-inflammatory-bowel-disease/
Consejo de Parásitos de Animales de Compañía (CAPC). (2025, 7 de febrero). Tricomoniasis. Obtenido de https://capcvet.org/guidelines/trichomoniasis/
PetMD. (s.f.). Los mejores probióticos para gatos. Obtenido de https://www.petmd.com/cat/vet-verified/best-cat-probiotics
IBDKitties.net. (sin fecha). Probióticos. Obtenido de https://www.ibdkitties.net/supplements/probiotics/
Manual veterinario Merck. (s.f.). Diferenciación de la diarrea del intestino delgado de la del intestino grueso. Obtenido de https://www.merckvetmanual.com/multimedia/table/differentiation-of-small-intestinal-from-large-intestinal-diarrhea
Capital Home Veterinary Care. (s.f.). 6 señales de que su gato necesita ver a un veterinario inmediatamente. Obtenido de https://www.capitalhomevetcare.com/blog/6-signs-your-cat-needs-to-see-a-vet-immediately/
Centro Veterinario Autumn Trails. (2023, 4 de diciembre). 5 tratamientos eficaces para la diarrea del gato. Obtenido de https://autumntrailsvet.com/5-effective-treatment-approaches-for-managing-cat-diarrhea/
Hospitales VCA. (s.f.). Pancreatitis en gatos. Obtenido de https://vcahospitals.com/know-your-pet/pancreatitis-in-cats
El Doctor Gato. (s.f.). Pancreatitis. Obtenido de https://thecatdoctor.co.uk/cat-health/pancreatitis/
Total.veter. (s.f.). ¿Cuáles son los mejores probióticos para gatos con diarrea?. Obtenido de https://total.vet/probiotics-for-cats-with-diarrhea/
Fondo Maddie. (sin fecha). Efectos del tratamiento probiótico en gatos que ingresan en un refugio. Obtenido de https://www.maddiesfund.org/probiotic-treatment-on-cats-entering-a-shelter.htm
MDPI. (s.f.). Impacto de Saccharomyces cerevisiae DSM 34246 (Canobios). Obtenido de https://www.mdpi.com/2306-7381/12/1/44#:~:text=boulardii%20plays%20a%20significant%20role,microbiota%20%5B1%2C5%5D.
Scribd. (s.f.). Tabla de puntuación fecal Purina. Obtenido de https://www.scribd.com/document/768462369/fecal-chart
VivaPets. (sin fecha). Estrés en los gatos: Síntomas, causas y tratamientos recomendados por el veterinario. Obtenido de https://vivapets.com/article/2428/stress-in-cats-symptoms-causes-and-vet-recommended-treatments
ExpertCatCare. (sin fecha). ¿Por qué tiene diarrea mi gato? Causas, diagnóstico y tratamiento. Obtenido de https://www.expertcatcare.com/article/why-does-my-cat-have-diarrhea-causes-diagnostics-treatment